- Home
- News & Features
- News
- FY2019
- 25 years since the Great Hanshin-Awaji Earthquake: Disaster medical assistance know-how and knowledge are passed on from the DMAT to the JDR (Part II)
News
January 17, 2020
25 years since the Great Hanshin-Awaji Earthquake: Disaster medical assistance know-how and knowledge are passed on from the DMAT to the JDR (Part II)
Mozambique, where the know-how of the two organizations functioned effectively
In March 2019, a massive cyclone hit the African eastern coast country of Mozambique. It was said to be the southern hemisphere’s worst-ever cyclone. In response to a request from the Government of Mozambique, a JDR team was quickly dispatched to the country.
 A JDR Medical Team member examines the victims in Mozambique and inputs patient information into the electronic medical record system
A JDR Medical Team member examines the victims in Mozambique and inputs patient information into the electronic medical record system
"To support the Mozambique Ministry of Health's Emergency Operation Center (EMTCC), a JDR Expert Team was dispatched to assist in the overall coordination of various international emergency medical teams. The team consisted of Japan's DMAT Secretariat members and public health experts who were at the heart of the development of the WHO-approved international standardization methodology MDS (Minimum Data Set). On the other hand, the JDR Medical Team, under the coordination of the EMTCC, developed medical care activities in areas where many evacuees had gathered but were unable to receive medical assistance. Those activities showed exactly how Japan's DMAT know-how was employed by the JDR overseas."
Above are the words of Dr. Tomioka Joji, who was dispatched to the disaster area as a deputy team leader and now chairs the Coordination Subcommittee of the JDR Medical Team. He has an anecdote that his experience of being affected by the Ebino Earthquake in 1968 sparked the initiative for his present medical activities.
 JDR Medical Team members operating water purifiers to provide safe medical care in the disaster-stricken areas of Mozambique. Dr. Tomioka is standing on the truck (photo on the right)
JDR Medical Team members operating water purifiers to provide safe medical care in the disaster-stricken areas of Mozambique. Dr. Tomioka is standing on the truck (photo on the right)
Dr. Tomioka then describes the history of the birth of J-SPEED, which consolidates the know-how of the JDR and the DMAT as follows.
"SPEED" (Surveillance in Post Extreme Emergencies and Disasters) was originally developed by the Philippine Ministry of Health and the WHO, to collect information on medical syndromes that become problematic in the event of a disaster. In order to prevent and control disease outbreaks and protect the health of disaster victims in the field of disaster medicine, real-time surveillance of the number of symptoms and signs reported by disaster victims is an important tool for decision-making. But, in the past disasters, the format and content of these reports varied among medical teams, making it difficult to compile data. This resulted in delays in grasping the overall situation, causing major issues.
At the time of the Typhoon Haiyan Disaster in the Philippines (2013), in an information coordination meeting (health cluster meeting), at the Foreign Medical Teams coordination meeting, Professor Kubo Tatsuhiko of Hiroshima University (Department of Public Health and Health Policy, Graduate School of Biomedical and Health Sciences), who participated as a JDR Medical Team member, made a proposal. He said, "The Philippines have a very simple reporting method using only a single A4-sized paper called SPEED. Why don't the international medical teams adopt this method?" The JDR Medical Team, led by Dr. Kubo, had been researching electronic medical record systems that can be used in the disaster-stricken areas for several years, and in the course of this research, they were aware of SPEED.
Fortunately, Dr. Kubo's proposal was accepted by teams from around the world. The teams adopted SPEED from the next day onward, demonstrating that problems related to health care in the disaster-stricken areas could be quickly and easily compiled and reflected in decision-making. We brought the reporting method back to Japan and improved it as J-SPEED for domestic use. When the Kumamoto Earthquake struck in 2016, many medical teams, including the DMAT, made use of it, which proved to be very effective. In addition, as a result of our recommendation to the WHO, J-SPEED became the international standard (MDS) in 2017, which was implemented for the first time in the aftermath of the Mozambique disaster in 2019, and achieved excellent results. SPEED, a local surveillance system in the Philippines, was globalized by the JDR Medical Team to become the international standard.”
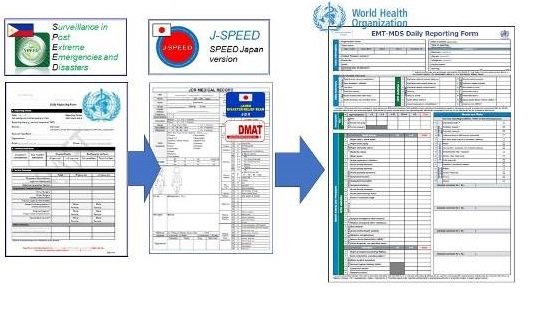 A daily report form using the MDS adopted by the WHO. The MDS is an internationally standardized system for data items that are extracted from medical records that must be reported to the coordination headquarters by medical teams working in the disaster-stricken areas in the event of a large-scale disaster. By immediately gathering accurate standardized data during the day’s treatment, health authorities can quickly and accurately make decisions based on the actual situation in the field, such as the deployment of medical teams and measures against infectious diseases
A daily report form using the MDS adopted by the WHO. The MDS is an internationally standardized system for data items that are extracted from medical records that must be reported to the coordination headquarters by medical teams working in the disaster-stricken areas in the event of a large-scale disaster. By immediately gathering accurate standardized data during the day’s treatment, health authorities can quickly and accurately make decisions based on the actual situation in the field, such as the deployment of medical teams and measures against infectious diseases
Issues in Japan's disaster medical care revealed during “3.11”
DMATs operating within Japan and JDRs for international disaster relief. A virtuous circle has been created by linking these organizations, either directly or indirectly, and each organization has been improving and evolving. However, some issues remain.
Take for example, "3.11." The Great East Japan Earthquake caused an unprecedented disaster in 2011. According to the National Police Agency, 18,428 people were killed or missing due to the earthquake (as of December 2019), and according to the Reconstruction Agency, 48,982 people still live as evacuees (as of November 2019).
 After the Great East Japan Earthquake struck, the DMAT immediately rushed to Hanamaki Airport (Iwate Prefecture), which served as a hub for wide-area medical transportation, and provided support to the victims
After the Great East Japan Earthquake struck, the DMAT immediately rushed to Hanamaki Airport (Iwate Prefecture), which served as a hub for wide-area medical transportation, and provided support to the victims
Looking back at the time, Dr. Koido, Director of the DMAT Secretariat, said, "In the Great East Japan Earthquake, more than 1,800 DMATs immediately entered the disaster-stricken areas and were able to respond to a variety of medical needs. On the other hand, in some cases, it was impossible through the DMAT to provide smooth transfer from hyperacute and acute phase emergency medical care to subacute or chronic phase general medical care. This resulted in a considerable number of disaster-related deaths."
This points out the importance of a system for checking the hygiene environment in evacuation centers and temporary housing following emergency medical care, and wide-ranging support with various occupations and fields for people requiring special attention in times of disaster, such as the elderly and patients with chronic diseases and dialysis.
"While we continue to improve DMAT skills, we urgently need to ensure that disaster response manuals, including the Business Continuity Plan (BCP) for disaster base hospitals and regional secondary medical institutions, are in place. In addition, the disaster medical coordinators, a system which was institutionalized after the Great East Japan Earthquake, worked vigorously after the Kumamoto Earthquake in 2016. But it is necessary to further enhance their activities."
Continuous challenges of the DMAT and the JDR
To prepare for the Nankai Trough and the Tokyo Metropolitan inland earthquakes, the national government, local governments, and private companies are currently implementing disaster prevention and mitigation measures such as building earthquake resistance and tsunami evacuation drills. From the perspective of disaster medicine, the two doctors talk about how the DMAT and the JDR should be in the future.
"As was the case in the Great East Japan Earthquake, in order to obtain overseas assistance when necessary, we need to quickly establish a procedure to accept medical teams from abroad that meets international standards, in accordance with the framework of international dispatch. Further training is also needed," says Dr. Tomioka.
Dr. Koido says, "We need to cultivate more world-class experts both in Japan and overseas. That is one reason why the JDR Medical Teams are participating in drills and training for the ‘ASEAN Regional Capacity on Disaster Health Management (ARCH) Project,’ which is currently underway with Southeast Asian countries. We must further promote disaster medical assistance from the point-to-line and line-to-surface perspectives. I feel that both Japan's JDR and DMAT have reached the top level in the world, but in terms of logistics both organizations still have room for improvement. These improvements include quickly allocating the necessary personnel, equipment, and supplies at the most appropriate time."
 JDR personnel participating in the training of the ASEAN Regional Capacity on Disaster Health Management (ARCH) Project held in Bali, Indonesia, in November 2019 (Dr. Koido is third from left in the rear row)
JDR personnel participating in the training of the ASEAN Regional Capacity on Disaster Health Management (ARCH) Project held in Bali, Indonesia, in November 2019 (Dr. Koido is third from left in the rear row)
It is said that there is no goal in disaster prevention. Both the JDR and the DMAT continue to learn from each other, aiming to "save as many lives as possible, no matter how difficult the situation may be."
Related Link
- About JICA
- News & Features
- Countries & Regions
- Our Work
- Thematic Issues
- Types of Assistance
- Partnerships with Other Development Partners
- Climate Change / Environmental and Social Considerations
- Evaluations
- Compliance and Anti-corruption
- Science and Technology Cooperation on Global Issues
- Research
- JICA Development Studies Program / JICA Chair
- Support for the Acceptance of Foreign HRs / Multicultural and Inclusive Community
- Publications
- Investor Relations