Towards TICAD8: Japan Promotes Universal Health Coverage in Africa
August 19, 2022
Japan has been playing a pivotal role in Africa's ongoing journey towards achieving universal health coverage (UHC), which is necessary to foster development, stability and resilience on the continent. The goal of UHC is to ensure that quality health services can reach everyone when needed, without incurring financial hardship.
UHC is a key area of focus that the Japan International Cooperation Agency (JICA) has been championing through the Tokyo International Conference on African Development (TICAD), which will convene in August for its eighth edition, hosted by Tunisia. While UHC is still a work in progress, it has already helped to reduce mortality rates and uplift communities across Africa.
"The fact that Japan has been leading TICAD with co-hosts such as the United Nations, the United Nations Development Programme (UNDP), World Bank and the African Union Commission (AUC), contributes to the UHC agenda in Africa, because it helps to refocus efforts on health by all the leadership in Africa," says Dr. Isabel MAINA, who heads healthcare financing at Kenya's Ministry of Health.

Dr. TOBE Makoto, Senior Advisor (health financing / health systems),
Human Development Department, Japan International Cooperation Agency (JICA)
Japan, whose UHC framework dates back to 1961, can serve as a good role model in areas such as the establishment of a national health insurance scheme and the management of a civil registry, and in its experience in infectious and lifestyle-related diseases, says Dr. TOBE Makoto, Senior advisor in the health sector at JICA.
In ensuring quality healthcare services, JICA has been helping African nations to build, upgrade, and renovate clinics, health centers, and hospitals; to train doctors, nurses, and midwives who can be dispatched to rural areas; and to procure medical equipment, drugs, and supplies.
In financial risk protection, Dr. Tobe adds that one huge barrier in healthcare access has been fear of high costs, amid perceptions that seeking medical help can plunge one into debt. What the UHC does is to shield, especially those in poverty, from making out-of-pocket payments.
"Many African countries are trying to establish a social health insurance system so that people don't have to pay a large amount out of pocket when they use health services, and they can enroll into health insurance before they get sick or injured," he says. "JICA is supporting African countries to establish a social insurance program, where payment is based on ability to pay (those who are able to pay for premiums pay while those who are not able to pay are cushioned) but access to services is based on need (i.e all can access services based on their needs regardless of whether they have paid for premiums or not)".
Such a continent-wide level of commitment among African leadership, Dr. Maina adds, has helped countries like Kenya move towards transitioning progressively from a heavy reliance on donor assistance, which can run dry, to more sustainable healthcare financing.

Dr. Isabel Maina Head, Health Financing, Ministry of Health, Kenya
Managing Diseases
The ongoing journey to UHC associated with economic growth has helped to reduce poverty, though this remains relatively high at about 43 per cent of households across Africa, Dr. Maina says. What may come to exact a toll on healthcare services is the prediction that the continental population will double to 2.5 billion people by 2050. Such demographic challenges means that the continent must prepare adequately and lay a good foundation for UHC and economic development.
Africa also faces the so-called "triple burden" of communicable diseases, non-communicable diseases, and injuries, though the composition of health threats varies by country. There are communicable or infectious diseases such as malaria and tuberculosis; non-communicable conditions such as diabetes, hypertension and cancers; as well as violence and injuries. For example, undernutrition remains a common problem in Sub-Saharan Africa but overweight and obesity are prevalent in North African countries, which suffer from cardiovascular diseases. Many other countries are still grappling with high levels of child and maternal mortality, while health systems are not able to deal with health threats.
JICA's focus on UHC, Dr. Tobe says, is intended to help Africa cope with emerging - and re-emerging - health threats, be they Ebola, malaria, monkeypox, polio, or COVID-19. This could be through top-down laboratory network development, or bottom-up grassroots and community efforts such as the distribution of mosquito nets to combat malaria.

Health personnel and JICA team visiting health facilities to learn best practices on flow of funds
to inform Public Finance Management (PFM) reforms
"The work we had done together with Japan before COVID helped to strengthen our health systems: this assured continued provision of essential health services during COVID and helped us to cope better post-COVID," Dr. Maina says. "COVID shook the entire system, but what was done before and with better planning has helped Africa to withstand the menace of the coronavirus."
Paying for Healthcare
It is also important to ensure that healthcare continues to be affordable for all, and that there is funding to build hospitals and train medical staff. Healthcare systems must be resilient to external shocks such as reduced donor funding or shifting priorities for the use of taxpayers' money among politicians.
Dr. Tobe, noting that it is difficult to look at improving healthcare without looking at where the funding will come from, says that this was an issue that many countries shied away from until 2010 when the World Health Organization shone a spotlight on financing.
"To purchase medicine, to upgrade health facilities and clinics, money is indispensable," Dr. Tobe says. "Donors can provide one-shot assistance on behalf of developing countries -- for example, JICA can donate a hospital using Japanese taxpayer money -- but to sustain this will require a consistent flow of money within the developing countries themselves."

Dr. TOBE Makoto having discussion with the Director General of the Senegalese Universal Health
Insurance Agency on cooperation by JICA (Photo owned by Dr. TOBE Makoto)
JICA has offered concessional loans at very low interest rates to countries such as Kenya, Cote d'Ivoire and Senegal, to support UHC initiatives such as ensuring financial access to health services for the poor and vulnerable population, or to increase the number of nurses and midwives in rural areas.
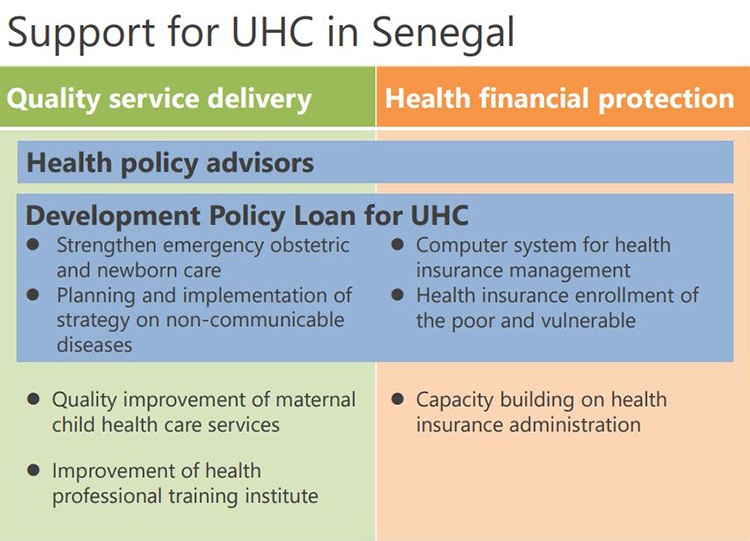
JICA's cooperation for UHC in Senegal (illustration made by Dr. TOBE Makoto)
Road towards UHC in Kenya
Dr. Maina notes that Kenya's road towards UHC is an ongoing journey that has been accelerated along the way together with stakeholders, including Japan's support.
Upon independence in 1963, the Government of Kenya committed to fight disease, poverty and illiteracy: a sure mix of moving towards UHC. In 1966, the National Hospital Insurance Fund was established to provide insurance for formal sector workers. Fast forward to 2013, when the Government initiated key programs towards UHC including the Linda Mama Programme (free maternity program); a health insurance subsidy for orphans and vulnerable children with support from JICA; an insurance subsidy for the elderly and persons with severe disabilities, other programs including insurance coverage for secondary school students (Edu Afya) as well as spirited efforts to strengthen health systems through inputs such as specialized equipment.
In 2017, UHC was identified as one of the "Big Four" Government agendas which culminated in a UHC pilot in four counties (sub national level) implemented through financing of inputs such as commodities, human resources for health, and equipment.
The lessons from the UHC pilot have informed the current UHC model through social health insurance implemented through a reformed National Health Insurance Fund into which all Kenyans must enroll. Dr. Maina says: "For those who can pay premiums, they will pay. For those who cannot pay, the government is supporting them with health insurance subsidies."
To further promote UHC's journey in Kenya and respond to the lessons from the UHC pilot, JICA offered an ODA loan to support implementation of UHC policy actions to Kenya. The areas of policy action were quite broad, such as public finance management reforms (eg budgetary management), quality of health services, health information, etc.
The progressive implementation of UHC has seen Kenya reap benefits as demonstrated by a few selected indicators, for example the Linda Mama Programme (free maternity services), has led to an increase in the percentage of health facility deliveries from 44 per cent in 2013 to nearly 80 per cent today. The deaths of children under 5 years of age has been remarkably reduced, from a high of 177 in 1963 to 42 per 1,000 live births in 2021 while life expectancy has increased from a low 49 years in 1963 to the current 67 years.
Ultimately, UHC means a healthier population that can support the economy, leading to a stable and more resilient society, Dr.Maina adds.
"UHC is about the entire being, the entire person. It is about the security of the people, the health of the people. Healthy people are able to contribute to the development of the country -- because if you're healthy, you're not in hospitals, you're able to go to your day-to-day work," Dr Maina says. "If your children are healthy, they're able to go to school. As a parent, you're able to go to work, and therefore the amount of money and time that would otherwise be spent on seeking health services, can contribute to economic development."
She adds: "People who are socially protected are more peaceful and unlikely to disturb the peace of the country. When there is peace, there is stability. A stable country is resilient because every aspect of the country, be it the economy, politics, society, is working."
Linking the three pillars of TICAD8: economy, society, and peace and stability, with UHC will help people better understand the importance of UHC.
Dr. Tobe concurs that healthy people are indispensable in economic development. Noting that no matter how rich or independent a person is, they tend to become more vulnerable as they get older or if their economic situation changes, he says: "A developed society enables support to the vulnerable on a society level, so that they are not dependent solely on their families. Unacceptable gaps in health make the world angry and unstable. UHC makes the world more peaceful and stable. "
TICAD8 is a good opportunity for African leaders to recognize the benefits and importance to investment in UHC for sustainable development of their countries, and for Japanese citizens to recognize how the world becomes more inter-dependent - what is happening in Africa influences on our daily lives in Japan. Supporting the development of Africa and UHC in Africa makes our daily lives in Japan more stable.
"A society with people who can support one another is one that can make the world more stable and more sustainable," Dr. Tobe says.
JICA supporting Side Events for "Health"