
A Ministry of Health administrator checks information sent to the mobile terminal.

mSOS logo
Used as an icon for promoting the system in Kenya
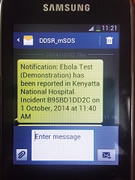
A situation report using the mSOS.
Technical cooperation in Kenya has helped establish an infectious disease rapid response system that utilizes cellular networks. The system uses common communication equipment and enables instant sharing of reports of infectious diseases even from small hospitals in developing countries.
Preventing the Spread of Epidemics with Mobile Phones
"If infectious diseases are not dealt with quickly, they can turn into epidemics," says Kouichi Morita, professor at Nagasaki University's Institute of Tropical Medicine. "Even minor cases in the countryside should be promptly and accurately reported to the central healthcare administration. In Kenya's rural areas, everyone from teenagers to tribal elders has access to a cell phone, so we came up with the idea of making an outbreak alert system using the cellular network." An experience in the World Health Organization (WHO) led Morita to turn his attention to cell phones. At that time, he was assigned to oversee immunization programs in the Pacific. He recalled that they ran out of vaccines one day. When on location, it is standard practice to report this situation to the center using a two-way radio. However, the radio was broken so they couldn't get through. Morita observed that many people had mobile phones, and the public nurses were more familiar with mobile phones than with radios. Moreover, mobile phones enabled data to be centrally organized, thus Morita thought that they were the best tool for the job.
Under the motto "early detection, early containment," Nagasaki University has been working with the Kenya Medical Research Institute (KEMRI) since 2012 to develop rapid diagnostic tests and outbreak alert systems for yellow fever and Rift Valley fever. The project, based at KEMRI's research facility, has been using new technology from Japan, and the tests and analyses of the system are shared by the two institutions. The University is also contributing toward project staff's professional development by inviting researchers for sabbaticals in Japan. In addition to staff training, simultaneous development of both diagnostic tests and an early detection system is underway. An outbreak alert system is vital, and it requires something cheap and familiar to everyone—a mobile phone fits the bill perfectly.
Convenient Enough to Use
Kenya has a system in which information is sent from local medical centers to county officers, who then report to the central health administration. A special form describing symptoms and other conditions must be filed. The process of organizing and analyzing the paperwork takes time. To overcome this time lag, Morita's team decided to develop an SMS reporting system (mSOS) that allows all suspected cases of a notifiable infectious disease to be reported using mobile phones instead of the usual paper forms. The reports sent via SMS immediately undergo epidemiological analysis and are then displayed at the Ministry of Health (MOH). The results are forwarded to an administrator at the Ministry and to local medical centers if necessary. This enables MOH personnel and local surveillance officers to head to the site immediately.
Nagasaki University dispatched Mitsuru Toda (now a PhD degree holder currently working at the CDC* in the US) to trial the network with the Kenyan MOH and medical centers in Nairobi County, Kajiado County, and Busia County in the western region bordering Uganda. She held lectures for local health professionals about surveillance using mSOS, distributed cell phones to be used for the system, and explained how the system and the cell phones operate. The participants' reactions were positive, and comments such as "The mSOS system is good because you can also receive replies for confirmation instead of just sending messages one-way." were often heard. The MOH representatives appreciated how information could be obtained in real time. The trial showed that when mSOS was not used, only 2.56% of infectious disease cases were reported, a striking contrast to the sevenfold (19.23%) increase of reported cases with the use of mSOS. In light of these results, the Kenyan MOH decided to officially adopt the system, and with the help of organizations such as UNICEF, the CDC, and the WHO, it is now being deployed throughout the country.
The ease of feeding accurate information into the system not only helps to prevent epidemics, but also makes it possible to formulate further measures by analyzing past data. If the system is successfully adopted in Kenya, it can be rolled out over the entire continent, and it would greatly help in the fight against the spread of infectious diseases.
*Centers for Disease Control and Prevention

A training seminar—which includes the operation of mSOS—held for public health professionals from various parts of Kenya.


mSOS data is organized for ease of viewing and displayed on the Internet.

Professor Kouichi Morita Institute of Tropical Medicine, Nagasaki University
Coordinator for Nagasaki University Graduate School of Biomedical Sciences Doctoral Leadership Program. Currently training future leaders in the fields of tropical medicine and emerging infectious disease control.




scroll