- Home
- Technical Cooperation Projects
- Index of Countries
- Africa
- Ghana
- Project for Improving Continuum of Care for Mothers and Children through the introduction of Combined MCH Record Book
- Project News
- Pilot test of the new combined MCH Record Book was conducted in Ghana
Project News
2018-04-30
Pilot test of the new combined MCH Record Book was conducted in Ghana
Background
Over the last decades, the Ghanaian health system has been employing two separate home-based records for maternal and child health, i.e. Maternal Health Records (MHR) and Child Health Records (CHR). The results of the Ghana Ensure Mothers and Babies Regular Access to Care (EMBRACE) Implementation Research Project (2012-16) highlighted the importance of linking MHR and CHR and educating mothers on the importance of continuum of care (CoC)[1] in order to promote CoC. In response to the recommendation, the Ministry of Health (MOH) and the Ghana Health Service (GHS) developed the combined Maternal and Child Health Record Book (MCH RB), an integrated home-based record for both mother and her child, with technical support from JICA. The book was designed to fill the gap of CoC and to encourage mothers and family members to take active roles in health and childcare.
Study Design
Prior to its national rollout, the MCH RB was piloted in the selected facilities in three regions (i.e. Ashanti, Central, and Upper West) from June 2017 to February 2018. The study aimed to examine expected comparative advantages of MCH RB over MHR and CHR. This quasi-experimental study was designed as a difference-in-difference (DID) study.
 Maternal Health Records (MHR) and Child Health Records (CHR)
Maternal Health Records (MHR) and Child Health Records (CHR)
 Combined Maternal and Child Health Record Book (MCH RB)
Combined Maternal and Child Health Record Book (MCH RB)
Selection of sites
A pair of districts in three regions (Ashanti, Central and Upper West) matched for socio-economic indicators was selected in each region to ensure homogeneity between them. Intervention and control facilities were randomly assigned in respective districts.
Intervention
The intervention group used MCH RB for six months, while the control group used MHR and/or CHR during the same period. Prior to the distribution of the MCH RB to women in the intervention group, 60 health workers working at interventions facilities participated in a two-day orientation on the contents of the MCH RB.


Study population
The panel consisted of 440 women in the intervention group and 442 women in the control group. Difference-in-difference (DID) linear regression models were primarily employed to examine the impact of the MCH RB.
Baseline and End line surveys
A structured interview was conducted using a questionnaire on knowledge, attitude and practice (KAP) and satisfaction with services. Baseline survey was conducted in June 2017. Follow-up survey was conducted with the same women who were involved in the baseline study in February 2018. A survey was also conducted for health workers (N=120) at the intervention facilities after the intervention. Data were collected using structured questionnaires and analyzed using STATA and SPSS.
Characteristics of respondents was examined utilizing the baseline data
Mean age of women between the intervention group (mean=26.63, sd=6.09) and the control group (mean=26.71, sd= 6.49), mean parity between the intervention group (mean=2.77, sd=1.70) and the control group (mean=2.60, sd=1.64), did not show a significant difference. While a majority of women completed lower secondary education (middle/junior high schools), approximately 30% women were illiterate in both groups. Marital status was different between the two groups, by showing significantly higher proportion of women either separated, divorced, or never married in the control group (7.5%) than intervention group (2.1%) (P < 0.001).
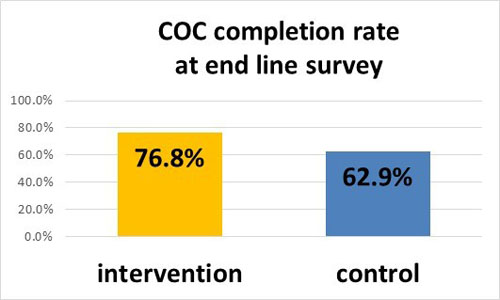
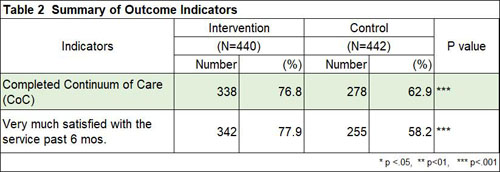
COC completion rate was higher in MCH RB users
In this study, CoC completion was defined as the utilizations of all key services: (i) ≥4 ANC visits; (ii) delivery assisted by skilled birth attendant; (iii) PNC within 48 hours after delivery, at two weeks and at six weeks for a mother and a child. CoC completion rate during last six months was significantly higher in the intervention group than in the control group at the time of follow-up (Intervention 76.8%, Control 62.9%, P < 0.001).
Knowledge was higher among MCH RB users
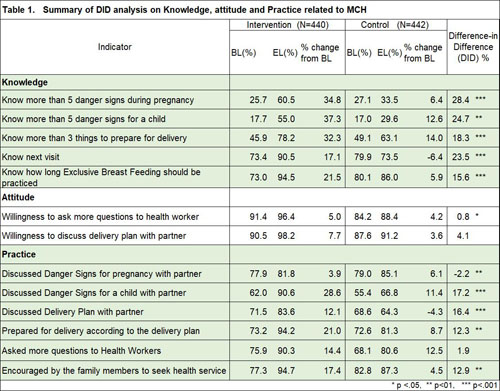
DID analyses confirmed that knowledge related to MCH were significantly higher in the intervention group than in the control group. The proportion of women having correctly identified more than five danger signs during pregnancy significantly increased more in the intervention group than in the control group (intervention from 25.7% to 60.5%, control from 27.1% to 33.5%, DID 28.4%, P < 0.001). Similarly, the proportions of women having correctly identified more than five danger signs during childhood (intervention from 17.7% to 55.0%, control from 17.0% to 29.6%, DID 24.7%, P < 0.01) and women having known more than three things to prepare for delivery (intervention from 45.9% to 78.2%, control from 49.1% to 63.1%, DID 18.3%, P < 0.001) significantly increased more in the intervention group than in the control group.
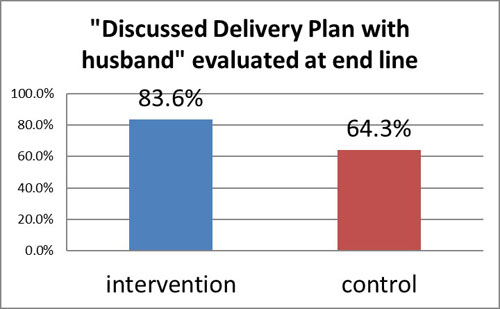
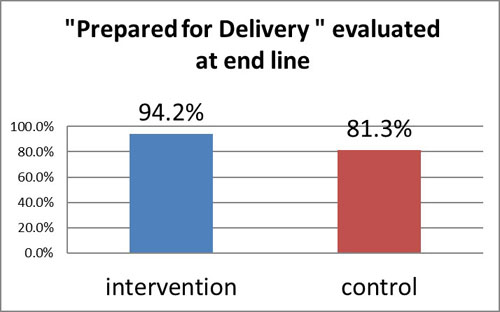
More communication and better preparation with the partner
Significantly greater proportions of couples in the intervention group discussed delivery plan (intervention from 71.5% to 83.6%, control from 68.6% to 64.3%, DID 16.4%, P < 0.001), and actually prepared for delivery (intervention from 73.2% to 94.2%, control from 72.6% to 81.3%, DID 12.3%, P < 0.01).
Higher Satisfaction among Women and Health Workers:
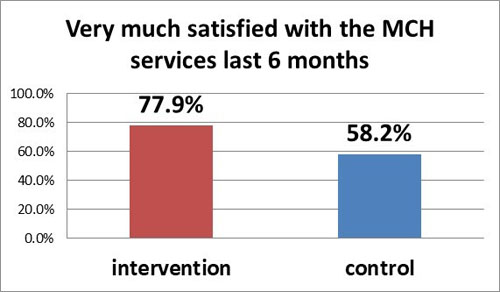
A significantly greater proportion of women having used MCH RB were "satisfied very much with the services last six months" at follow-up (Intervention 77.9%, Control 58.2%, P < 0.001). Eighty-six percent of health workers having used MCH RB agreed that the MCH RB made their works more efficient than two separate records, 97% of them thought that MCH RB helped them provide better health services, while 73% felt their work might have become busier. This may be because health workers needed to transcribe the data from the MHR and CHR to MCH RB.

Conclusion
The findings of the study confirmed that use of the MCH RB is likely to promote CoC by raising awareness on and preparation for MCH-related risks, and by encouraging women to seek essential services. The MCH RB is also highly accepted by both women and health workers, while the extra duty of the health workers during the transition period from the two separate records to the integrated home-based record need to be carefully considered with supportive measures in the actual implementation for the national program. Based on the results of this piloting, the Ghanaian MOH launched the MCH RB for nationwide scaling-up, in March 2018.
Note
- [1] Continuum of Care is a series of reproductive, maternal, new-born and child health care, including antenatal care (ANC), delivery with assistance of skilled birth attendant, prenatal care (PNC) and child growth and development check.
- About JICA
- News & Features
- Countries & Regions
- Our Work
- Thematic Issues
- Types of Assistance
- Partnerships with Other Development Partners
- Climate Change / Environmental and Social Considerations
- Evaluations
- Compliance and Anti-corruption
- Science and Technology Cooperation on Global Issues
- Research
- JICA Development Studies Program / JICA Chair
- Support for the Acceptance of Foreign HRs / Multicultural and Inclusive Community
- Publications
- Investor Relations
